Attracting clinical trials to Norway

Dr. Jon Amund Kyte at Oslo University Hospital (OUH) and Oslo Cancer Cluster share the common goal of bringing more clinical trials to Norway.
Jon Amund Kyte is the new Head at the Department of Experimental Cancer Treatment at OUH. He also runs three separate clinical trials and is the leader of a research group at the Department of Cancer Immunology, where he develops novel CAR T cell therapy and conducts translational studies.
Kyte aims to increase the number of and improve the quality of clinical trials in Norway. He says this will contribute to more patients gaining access to novel cancer treatments and to improving the efficacy of cancer therapies.
“The only way to improve cancer treatment is to have clinical trials,” said Kyte.
Oslo Cancer Cluster also wants to bring more clinical trials to Norway to develop innovative cancer medicines. The ambition is to enable faster patient recruitment from across the Nordic region, so that many more can benefit from new treatments, such as immunotherapy.
Promising advances
Immunotherapy represents a new type of cancer treatment, which activates the patient’s immune-system to fight off the cancer cells. It gives doctors the opportunity to help patients that previously had limited treatment options. Most types of immunotherapy also cause less side effects than traditional cancer treatments.
“The important point is that immunotherapy can have a long-term effect,” said Kyte.
“Most patients that experience a recurrence or progression of the disease cannot be cured. The traditional treatments only have a limited, short-term effect on them. But immunotherapy may have a long-term effect on the patient – and, in some cases, even cure the disease.”
Two big challenges
Immunotherapy may sound like a miracle drug, but researchers still have a long way to go to perfect the treatment for all cancer patients. Kyte highlights two of the biggest barriers that remain.
“One challenge is to develop immunotherapy so that it works efficiently on all types of cancer. The other challenge is to learn how to choose personalised treatment plans: to identify an individual’s biomarkers and find out which treatment will be effective for that specific patient.”
A biomarker is a biological molecule in the patient’s body and these may be used to see how well a patient will respond to a certain treatment. Kyte said that to develop immunotherapy, there needs to be more clinical trials. It is the only way for researchers to find out how to activate an immune response in the patient’s body.
“A big potential for development lies in trying different possible combinations of cancer treatments. In my clinical trials, for example, we combine immunotherapy with immunogenic chemotherapy or radiation therapy,” Kyte explained.
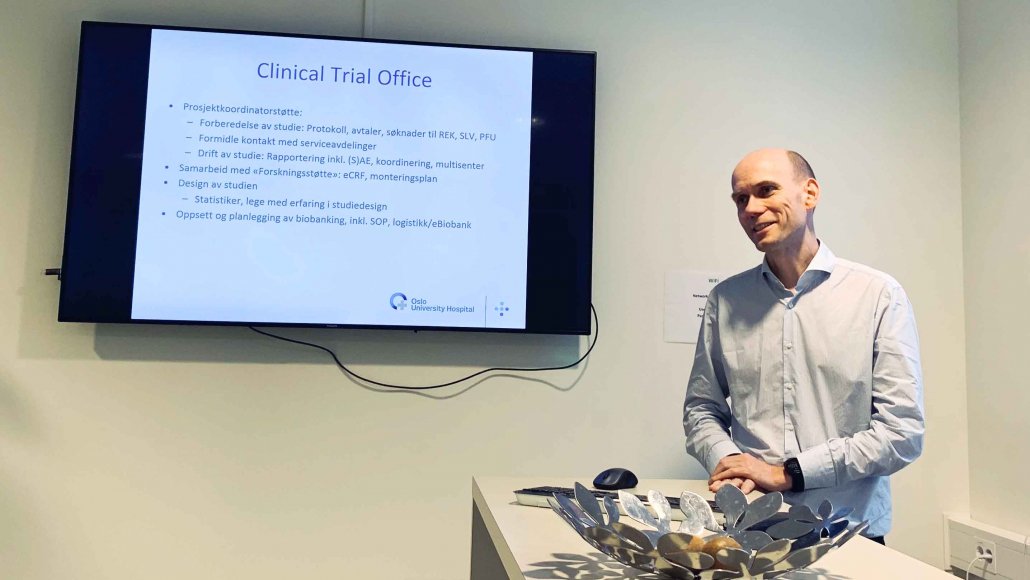
The Clinical Trial Unit are experts in assisting companies and researchers to conduct clinical trials in Norway.
Welcome, companies
OUH has a long history of conducting clinical trials and is an appealing option for both researchers, doctors and companies that wish to initiate their own trials. Kyte welcomes more companies to conduct clinical trials at OUH:
“The more clinical trials that are conducted here by companies, the stronger our clinical research environment becomes and our ability to run our own studies is also strengthened.”
The Clinical Trial Unit in Kyte’s department offers its services to companies that want to run a clinical trial at OUH. They have extensive background knowledge of how the hospital is organised and which approvals are needed to conduct a clinical trial in Norway. They can step in as project coordinator for companies that need help to get their clinical trials up and running.
“We are highly experienced in applying for approvals in Norway. When you run a clinical trial, there are regulations from the Norwegian Medicines Agency and the ethical committee and other governmental agencies. A clinical trial also involves many different parts of the hospital – the departments of pathology and radiology, the laboratories, the infusion unit, the hospital wards and out-patient clinic and the administrative offices that oversee different agreements, data management and biobanking.”
Nordic clinical trials
All these administrative obstacles may appear discouraging, but there are many convincing reasons to conduct a clinical trial in Norway.
“The Oslo University Hospital is a good place to run a clinical trial, because in terms of the number of cancer patients, it is one of the largest hospitals in Europe. Norwegian healthcare is also extremely well-organised. Patients are rarely lost to follow-up, because there are no private healthcare alternatives and patients rarely move out of the country,” Kyte explained.
The Clinical Trial Unit is also taking part in the development Nordic Nect, a collaboration to recruit patients from the entire Nordic region to clinical trials. The plan is to have one hospital where the clinical study is conducted and to involve patients from Sweden, Denmark, Finland and Norway. There will then be a population of 25 million people from which to recruit patients, which opens the possibility for larger clinical trials.
“This is a good thing for the companies that want to run clinical trials in Norway. It is also good for the researchers. But most of all, it is good for the patients – who have the opportunity to take part in more novel cancer treatments,” said Kyte.
- To learn more about the Clinical Trial Unit, please visit their website.
- Need help to get your clinical trial started? Get in touch with the Department of Experimental Cancer Treatment.










